INTRODUCTION
In the United States, 17 people on the waiting list for an organ transplant die each day (1). In 2021, the number of kidney transplants performed (24,670) was approximately 27% of the total number of people on the waiting list (90,483) (1). As of 2020, 17.6% of people on the heart transplant list and 31.1% of people on the kidney transplant list had been waiting for three years or more (2, 3). Therefore, there is a significant shortage of organs available for transplantation.
Xenotransplantation has been suggested to be the most feasible and promising answer to the organ shortage (4-6). Instead of relying on human donors, genetically engineered pigs can theoretically provide an unlimited source of organs, greatly reducing or even solving the organ shortage. It would also eliminate the morbidity and mortality associated with long stays on transplant waiting lists and decrease healthcare costs associated with sustaining patients waiting for transplant (6). However, xenotransplantation is still a technology in development, with great aspirations, but minimal clinical success thus far. Recent advances suggest that xenotransplantation is poised to make the jump into clinical trials, but controversies about the logistics and ethics of such trials abound. This review will survey the history, recent advances, and ethical controversies surrounding xenotransplantation, with a focus on cardiac and renal xenotransplantation.
HISTORY OF XENOTRANSPLANTS
Early xenotransplantation was intertwined with the initial development of allotransplantation. In the 1960s, when renal allotransplantation was in its infancy, Keith Reemstma and Thomas Starzl both attempted renal xenotransplantation using chimpanzee and baboon, respectively, as donors (7, 8). These transplants were largely unsuccessful, with most patients dying within days of the transplant. The limited methods of immunosuppression available – azathioprine, prednisone, actinomycin C, and local irradiation – were insufficient in some patients to prevent rejection and caused severe infections in others (7, 8). In 1964, three years before the first modern human heart allotransplant, James Hardy attempted the xenotransplantation of a chimpanzee heart, which survived for less than an hour9. In 1985, xenotransplantation came to increased public attention with the transplant of a baboon heart into neonate with hypoplastic left heart syndrome, “Baby Fae”. Treated with cyclosporine, she survived for 20 days post-transplant, dying due to graft necrosis as well as lung and kidney failure (10).
By the 1990s, xenotransplantation research mainly focused on pigs as the optimal donors, because of their easy availability for breeding and reasonably concordant size and physiology (11, 12). While xenotransplants sourced from non-human primates posed a lower immunological risk of rejection, practicality concerns about breeding primates in large numbers, potentially discordant organ size, and public acceptance of breeding primates to harvest organs prevented their use (11, 12). Pigs were easily bred and appropriately sized alternatives that were already farmed in large numbers for human use.
When initially attempted, early pig xenotransplants in the 1990s led to immediate hyperacute rejection as a reaction to xenoantigens present on porcine cells (12). Around this time, Uri Galili discovered the α-galactosyl epitope (α-gal), which was determined to be the main xenoantigen responsible for hyperacute rejection (13, 14). Humans, apes, and Old World monkeys do not produce α-gal, while New World monkeys and non-primate mammals do (13). Approximately 1% of human B cells produce antibodies against α-gal (anti-Gal) and the IgG anti-Gal titer increases 100-fold in the two weeks following exposure to a xenograft (13). This strong immunological response made controlling hyperacute rejection by immunosuppression very difficult, and thus attention turned to the genetic modification of pig donors to minimize the issue. The first α-1,3-galactosyltransferase homozygous knockout pigs (GTKO) were developed in 2003 using nuclear transfer cloning technology (15, 16). Early experiments using GTKO pigs as donors for xenotransplantation in a primate model showed significantly improved success, with xenografts surviving for a median time of 78 days (17). In comparison, xenografts from pigs engineered to express low levels of α-gal were universally rejected within 20 minutes (17). The development of GTKO pigs was a major advancement and ushered in the modern era of xenotransplantation research.
RECENT ADVANCES
Animal Models
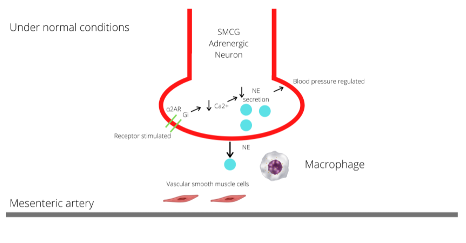
In the two decades since the development of GTKO pigs, modern xenotransplantation research has focused on further genetic modification of porcine donors, as well as optimizing the immunosuppression regime necessary to maintain graft survival in primate models. The use of CRISPR/Cas9 allows researchers to insert a large number of modifications into the genome with much greater speed and precision (18). This has facilitated the proliferation of multiple genetic modifications tested in animal models of xenotransplantation. The wide variety of genetic modifications attempted has been reviewed elsewhere (19). In brief, while GTKO pigs greatly improved the risk of hyperacute rejection, complement activation and dysregulation of the coagulation cascade still impaired graft survival, even in the absence of antibody binding (19-22). Common genetic modifications to address these issues include the insertion of human complement regulatory transgenes, such as CD46 or CD55, and human coagulation regulatory transgenes, such as thrombomodulin (19-23). Two additional xenoantigens have been discovered to also play an important role in the immunological reaction to xenografts: N-glycolylneuraminic acid and the Sda blood group antigen (19).
Genetic modification of donor animals is only one aspect of efforts to sustain a xenograft. While the eventual goal would be sufficient genetic modification to eliminate the need for immunosuppression post-transplant, currently significant immunosuppression is necessary. Recent experiments in animal models have employed a combination of conventional immunosuppressants used in allotransplants, including anti-thymocyte globulin, rapamycin, corticosteroids, mycophenolate mofetil, and anti-CD20 antibody (21, 24-29). The addition of a costimulation blockade via anti-CD40 or anti-CD154 antibodies significantly improves graft survival along with the conventional regimen (21, 24-29).
These innovations have allowed for the prolonged survival of xenografts in primate models. Kim et al. regularly sustained renal xenografts for a year, with several surviving for up to 400 days using monoclonal antibody depletion of CD4+ T cells (30). In other experiments, renal xenografts repeatedly lasted over 120 days, with the longest survival times of 7, 8, and 10 months (32-34). Heterotopic cardiac xenografts have a median survival of 298 days, with the longest survival being 945 days (29). Orthotopic cardiac xenografts, which are a more challenging model to sustain, have repeatedly lasted up to three months, with the longest survival of 195 days (23). These results demonstrate that research has begun to reach the standards for clinical trial initiation set by the Xenotransplantation Advisory Committee of the International Society for Heart and Lung Transplantation (6).
Human Models
Given these promising results in animal models, initial attempts have been made at solid organ xenotransplantation in humans. In three instances, porcine kidneys were transplanted into human recipients who were declared brain-dead and who were ineligible to serve as organ donors (31, 32). The model of a brain-dead human recipient is limited, because the environment created by brain death may affect xenograft function, and the nature of the experiment prevents long-term follow-up (31, 32). In particular, these experiments were criticized because of their time-limited nature and the difficulty of interpreting physiologic parameters post-transplant because the recipients’ kidneys were not removed33. However, this work can still provide valuable initial data as a stepping stone to a clinical trial, without many of the risks and ethical quandaries of a clinical trial. In all three instances, the kidneys remained viable and produced urine throughout the 54- or 72-hour follow-up period, with no evidence of hyperacute rejection or antibody mediated injury (31, 32).
In early 2022, researchers at the University of Maryland performed the first transplant of a genetically modified pig heart into a living human with the possibility of recovery (33, 34). While the UMD team was denied authorization for a full clinical trial of cardiac xenotransplantation, the Food and Drug Administration granted an authorization for compassionate use in the case of a 57-year-old man who was ineligible for mechanical support devices or an allotransplant and had been dependent on venoarterial extracorporeal membrane oxygenation (ECMO) for two months (33, 34). The transplanted pig heart had 10 genetic modifications: knockout of the three main pig xenoantigens and 6 modifications to minimize the immune response. The patient received B- and T-cell depleting therapies, anti-CD40, and additional immunosuppressive therapies (34).
The xenograft showed normal cardiac function, and the patient demonstrated clinical improvement in the first seven weeks post-transplant. At the seven-week mark, the patient started to deteriorate significantly, and the graft showed diastolic failure and myocardial thickening, although the systolic function was preserved (34). Supportive care was withdrawn 60 days after transplantation. Throughout this process, no evidence of acute cellular or antibody-mediated graft rejection was observed. The mechanism for the pathologic changes observed in the graft are unexplained at this time. This is additionally complicated by the detection of porcine cytomegalovirus and human herpesvirus 6 in the patient’s later tests, although the donor animal initially screened negative for cytomegalovirus (34). Overall, the patient’s initial progress and recovery, as well as the life-sustaining nature of the porcine graft are promising results for the field of xenotransplantation. However, this experience also emphasizes that there are still important gaps in the knowledge about xenotransplantation.
ETHICAL CONTROVERSIES
Xenotransplantation sparks a multitude of ethical questions, including but not limited to the appropriate use of animals, acceptability from a religious perspective, the utility of investing in xenotransplant, the infectious disease risk, and the design of an eventual clinical trial. The choice of pigs as the source animals for xenografts effectively minimizes concerns regarding animal use and animal rights. Pigs are farmed by millions as a food source and are already used in medical settings as sources of heart valves and insulin (35, 36). Individuals or communities may object to the use of pigs in this manner. As this is not a widely held belief, it does not constitute a sufficiently strong objection to impede further progress in xenotransplantation research (35, 36). Regarding religion, Christian, Jewish, and Muslim theologians have written about the acceptability of xenotransplant (37-40). While teachings of Judaism and Islam prevent the consumption of pork, theologians have deemed porcine xenotransplant acceptable given the primacy of preserving human life in both religions (37-40). However, this does not exclude the possibility that individuals may decide against a xenotransplant on these grounds. Thus, in both the case of animal use and the question of religious acceptability, overarching systemic beliefs support xenotransplant. However, individual beliefs about these topics may affect the choices made by future patients regarding whether to accept a xenotransplant.
The significant resource investment necessary to develop any new technology such as xenotransplantation should be examined carefully to ensure its worth. The dedication of resources towards xenotransplant research compared to prevention, nonsurgical treatments, or other emerging technologies for organ replacement is a decision to be made by governments individually, based on societal and cultural beliefs and standards. However, as described earlier in this review, there is a clear and pressing need to address the shortage of organs, and xenotransplantation is one of the technologies closest to clinical application that could remedy this issue. In the ideal future, transplant surgery would be nearly obsolete, because prevention measures and medical treatments will have advanced to the point that very few patients end up in organ failure. However, this utopia is likely to be unobtainable for decades, if ever. Recent trends, such as the 243% increase in patients on transplant waiting lists from 1991 to 2001, suggest that the pressing organ shortage is more likely to worsen than improve (4). In addition, improvements in medical care that improve lifespan may also increase the need for organ transplants to address age-related decline in organ function (18). There may also always be cases that require transplants, such as congenital organ defects. The potential benefit of xenotransplantation in providing an unlimited source of organs in these cases should not be overlooked (41).
Infectious disease risk and the design of future xenotransplant clinical trials are more complicated ethical questions. In a world still reeling from the COVID-19 pandemic, the risk of spreading new zoonotic infections via xenotransplantation should not be underestimated. Potential culprits include porcine cytomegalovirus, porcine endogenous retroviruses (PERVs), and other porcine microbes. Much of the concern around zoonotic transmission centers on PERVs, because the risk of other infections can be minimized, but not eliminated, by raising donor animals in specific pathogen free environments, repeated testing, and other infection control measures (35, 42, 43). In addition, there are concerns that PERVs, like other retroviruses, could cause malignancies or immunodeficiency when introduced to human hosts. However, the evidence thus far in primate models as well as the monitoring of humans exposed to pig tissues suggests that the risk of PERV transmission is extremely low (44-47). This evidence does not entirely ameliorate concerns, as it is possible that immunosuppressed conditions of solid organ xenotransplantation in humans could increase the likelihood of PERV transmission and replication. One possibility is to use animals in which PERVs were inactivated in the genotype (48). However, it is not clear whether investment in developing these animals with the necessary genetic modifications is worthwhile given the seemingly low risk. There is also the additional concern of introducing genomic instability by inactivating all PERVs in the genotype, given that there are approximately 25 copies of PERV in genomic DNA (48).
Each government needs to make its own determination about the severity of the infection risk inherent in xenotransplantation. However, given the large stake that society has in preventing new zoonotic infections, evaluation of this issue warrants special care. Citizen panels and public discussion after education on the topic should be considered so that a wide variety of opinions are weighed and to ensure that this decision is not made in an ivory tower (49). In addition, the COVID-19 pandemic has clearly demonstrated the inherent global interest in preventing the spread of new zoonotic infections. As such, even though it is reasonable that different nations may have varying levels of risk tolerance regarding the infection risk, it is critical that all nations pursuing xenotransplantation research do so while following accepted guidelines for minimizing infection risk. International bodies such as the World Health Organization can help encourage adherence to such practices, even if there is no way to mandate it.
One practice that has been proposed to minimize infection risk is to require that all participants in a future xenotransplant clinical trial be closely evaluated for infection for the rest of their lives (50, 51). This is a troubling requirement from an ethical perspective, as it violates a fundamental right of clinical trial participants outlined in the Declaration of Helsinki – to withdraw from the trial at any time (49, 52). The necessity of lifelong surveillance has been challenged recently, but remains a consensus guideline for future clinical trials (53). Ultimately, it is reasonable that early xenotransplantation clinical trials begin with the intention of lifetime surveillance, a requirement that could then be reduced or increased depending on the new data collected. Building this lifetime surveillance into future clinical trials means that the Declaration of Helsinki cannot be applied to its fullest extent (52). This should be clarified to any potential participant as part of the informed consent process. In addition, this may preclude early trials of pediatric xenotransplantation. Even though neonatal heart xenotransplantation may be one of the most promising early applications of clinical xenotransplantation, committing pediatric patients to lifetime monitoring would be overly problematic from an ethical perspective (41, 54, 55).
Much has been written about the design of a potential xenotransplant clinical trial, specifically on the appropriate patient population (35, 41, 52, 54-56). The specific indications favored for trial inclusion vary, but the consensus is that initial trial participation should be limited to those who are highly unlikely to receive an allotransplant and who are both medically and psychosocially healthy enough to maximize the chances of a successful transplant (35, 41, 52, 54-56). However, it remains a challenging task to balance the need for xenotransplantation research done in humans with the risk of taking advantage of vulnerable and desperate patient populations, especially given that there is no guarantee that initial trials of xenotransplantation will have significant clinical success.
DISCUSSION
Xenotransplantation research appears to be at an important crossroads, as it teeters from preclinical models into clinical trials. Recent advances in preclinical models have demonstrated significant success, and the potential benefits of clinical xenotransplantation are tremendous. However, transitioning into clinical trials is an especially difficult proposition, given that so much remains unknown about this technology. Recent attempts at xenotransplantation in humans highlight that there are still major gaps in our knowledge. Fully addressing these gaps will require clinical trials. Additionally, a clinical trial, rather than additional case studies, would be better poised to address ethical concerns and produce generalizable data on the genetic modifications and immunosuppression regimen necessary to sustain a xenograft. Therefore, it is reasonable to proceed with small early clinical trials in the near future, and reports from the Food and Drug Administration in July 2022 suggest that these trials may soon be on the horizon in the United States58. However, the regulation of these trials may require modification of existing standards. For example, adapting the standards for approval of genetic modifications may be necessary, as many of these transgenes have only been tested in combination, which makes determining the individual benefit of each construct difficult59. In addition, requirements for lifetime monitoring for infectious disease risk threaten long-held ethical standards, but a shift in these standards may be necessary to pursue the incredible benefit offered by xenotransplantation in the clinical world.
DISCLOSURES
Funding: Not applicable.
Conflicts of interest: None.
Availability of data and materials: Not applicable.
Code availability: Not applicable.
Authors’ contributions: Authors listed in the manuscript have contributed per submission guidelines and standards for authorship.
Ethics approval: Not applicable.
Consent to participate: Not applicable.
REFERENCES
1. Organ Procurement and Transplantation Network. Organ Donation Statistics. Health Resources & Services Administration; 2022. (Accessed June 20, 2022 at https://www.organdonor.gov/learn/organ-donation-statistics)
2. Colvin M, Smith JM, Ahn Y, et al. OPTN/SRTR 2020 Annual Data Report: Heart. Am J Transplant. 2022;22 Suppl 2:350-437.
3. Lentine KL, Smith JM, Hart A, et al. OPTN/SRTR 2020 Annual Data Report: Kidney. Am J Transplant. 2022;22(S2):21-136.
4. Ekser B, Cooper DKC, Tector AJ. The need for xenotransplantation as a source of organs and cells for clinical transplantation. Int J Surgery. 2015;23:199-204.
5. Mou L, Chen F, Dai Y, et al. Potential alternative approaches to xenotransplantation. Int J Surgery. 2015;23:322-326.
6. Cooper DKC, Keogh AM, Brink J, et al. Report of the xenotransplantation advisory committee of the international society for heart and lung transplantation. J Heart Lung Transplant. 2000;19(12):1125-1165.
7. Reemtsma K, Mccracken BH, Schegel JU. Renal Heterotransplantation in Man: Ann Surg. 1964;160(3):384-410.
8. Starzl TE, Marchioro TL, Peters GN, et al. Renal Heterotransplantation from Baboon to Man: Experience with 6 Cases. Transplantation. 1964;2(6):752-776.
9. Hardy JD, Kurrus FD, Chavez CM, et al. Heart Transplantation in Man. Developmental Studies and Report of a Case. JAMA. 1964;188:1132-1140.
10. Bailey LL, Nehlsen-Cannarella SL, Concepcion W, Jolley WB. Baboon-to-human cardiac xenotransplantation in a neonate. JAMA. 1985;254(23):3321-3329.
11. Cozzi E, White DJG. The generation of transgenic pigs as potential organ donors for humans. Nat Med. 1995;1(9):964-966.
12. Taniguchi S, Cooper DK. Clinical xenotransplantation: past, present and future. Ann R Coll Surg Engl. 1997;79(1):13-19.
13. Galili U. Interaction of the natural anti-Gal antibody with α-galactosyl epitopes: a major obstacle for xenotransplantation in humans. Immunol Today. 1993;14(10):480-482.
14. Oriol R, Ye Y, Koren E, et al. Carbohydrate antigens of pig tissues reacting with human natural antibodies as potential targets for hyperacute vascular rejection in pig-to-man organ xenotransplantation. Transplantation. 1993;56(6):1433-1442.
15. Lai L, Kolber-Simonds D, Park KW, et al. Production of α-1,3-Galactosyltransferase Knockout Pigs by Nuclear Transfer Cloning. Science. 2002;295(5557):1089-1092.
16. Phelps CJ, Koike C, Vaught TD, et al. Production of α1,3-Galactosyltransferase-Deficient Pigs. Science. 2003;299(5605):411-414.
17. Kuwaki K, Tseng YL, Dor FJMF, et al. Heart transplantation in baboons using α1,3-galactosyltransferase gene-knockout pigs as donors: initial experience. Nat Med. 2005;11(1):29-31.
18. Platt JL, Cascalho M. The Future of Transplantation. N Engl J Med. Published online June 22, 2022:NEJMe2207105.
19. Cooper DKC, Hara H, Iwase H, et al. Justification of specific genetic modifications in pigs for clinical organ xenotransplantation. Xenotransplantation. 2019;26(4).
20. Azimzadeh AM, Kelishadi SS, Ezzelarab MB, et al. Early graft failure of GalTKO pig organs in baboons is reduced by expression of a human complement pathway-regulatory protein. Xenotransplantation. 2015;22(4):310-316.
21. Iwase H, Ekser B, Satyananda V, et al. Pig-to-baboon heterotopic heart transplantation - exploratory preliminary experience with pigs transgenic for human thrombomodulin and comparison of three costimulation blockade-based regimens. Xenotransplantation. 2015;22(3):211-220.
22. Cooper DKC, Ezzelarab M, Iwase H, Hara H. Perspectives on the Optimal Genetically Engineered Pig in 2018 for Initial Clinical Trials of Kidney or Heart Xenotransplantation. Transplantation. 2018;102(12):1974-1982.
23. Längin M, Mayr T, Reichart B, et al. Consistent success in life-supporting porcine cardiac xenotransplantation. Nature. 2018;564(7736):430-433.
24. Higginbotham L, Mathews D, Breeden CA, et al. Pre-transplant antibody screening and anti-CD154 costimulation blockade promote long-term xenograft survival in a pig-to-primate kidney transplant model. Xenotransplantation. 2015;22(3):221-230.
25. Iwase H, Liu H, Wijkstrom M, et al. Pig kidney graft survival in a baboon for 136 days: longest life-supporting organ graft survival to date. Xenotransplantation. 2015;22(4):302-309.
26. Iwase H, Hara H, Ezzelarab M, et al. Immunological and physiological observations in baboons with life-supporting genetically engineered pig kidney grafts. Xenotransplantation. 2017;24(2):e12293.
27. Mohiuddin MM, Corcoran PC, Singh AK, et al. B-Cell Depletion Extends the Survival of GTKO.hCD46Tg Pig Heart Xenografts in Baboons for up to 8 Months: Anti-CD20 Mediate Long-Term Xenograft Survival. Am J Transplant. 2012;12(3):763-771.
28. Mohiuddin MM, Singh AK, Corcoran PC, et al. Role of anti-CD40 antibody-mediated costimulation blockade on non-Gal antibody production and heterotopic cardiac xenograft survival in a GTKO.hCD46Tg pig-to-baboon model. Xenotransplantation. 2014;21(1):35-45.
29. Mohiuddin MM, Singh AK, Corcoran PC, et al. Chimeric 2C10R4 anti-CD40 antibody therapy is critical for long-term survival of GTKO.hCD46.hTBM pig-to-primate cardiac xenograft. Nat Commun. 2016;7(1):11138.
30. Kim SC, Mathews DV, Breeden CP, et al. Long‐term survival of pig‐to‐rhesus macaque renal xenografts is dependent on CD4 T cell depletion. Am J Transplant. 2019;19(8):2174-2185.
31. Porrett PM, Orandi BJ, Kumar V, et al. First clinical‐grade porcine kidney xenotransplant using a human decedent model. Am J Transplant. 2022;22(4):1037-1053.
32. Montgomery RA, Stern JM, Lonze BE, et al. Results of Two Cases of Pig-to-Human Kidney Xenotransplantation. N Engl J Med. 2022;386(20):1889-1898.
33. Reardon S. First pig-to-human heart transplant: what can scientists learn? Nature. 2022;601(7893):305-306.
34. Griffith BP, Goerlich CE, Singh AK, et al. Genetically Modified Porcine-to-Human Cardiac Xenotransplantation. N Engl J Med. Published online June 22, 2022:NEJMoa2201422.
35. Sykes M, d’Apice A, Sandrin M, IXA Ethics Committee. Position paper of the Ethics Committee of the International Xenotransplantation Association. Transplantation. 2004;78(8):1101-1107.
36. Smetanka C, Cooper DKC. The ethics debate in relation to xenotransplantation. Rev Sci Tech. 2005;24(1):335-342.
37. Sautermeister J, Mathieu R, Bogner V. Xenotransplantation-theological-ethical considerations in an interdisciplinary symposium. Xenotransplantation. 2015;22(3):174-182.
38. Ebner K, Ostheimer J, Sautermeister J. The role of religious beliefs for the acceptance of xenotransplantation. Exploring dimensions of xenotransplantation in the field of hospital chaplaincy. Xenotransplantation. 2020;27(4).
39. Mathieu R. Jewish ethics and xenotransplantation. Xenotransplantation. 2016;23(4):258-268.
40. Padela AI, Duivenbode R. The ethics of organ donation, donation after circulatory determination of death, and xenotransplantation from an Islamic perspective. Xenotransplantation. 2018;25(3):1-12.
41. Cleveland D, Adam Banks C, Hara H, et al. The Case for Cardiac Xenotransplantation in Neonates: Is Now the Time to Reconsider Xenotransplantation for Hypoplastic Left Heart Syndrome? Pediatr Cardiol. 2019;40(2):437-444.
42. Denner J. Xenotransplantation and porcine cytomegalovirus. Xenotransplantation. 2015;22(5):329-335.
43. Knoll MF, Cooper DKC, Bottino R. How the COVID-19 pandemic may impact public support for clinical xenotransplantation in the United States? Xenotransplantation. 2020;27(5):e12623.
44. Paradis K, Langford G, Long Z, et al. Search for Cross-Species Transmission of Porcine Endogenous Retrovirus in Patients Treated with Living Pig Tissue. Science. 1999;285(5431):1236-1241.
45. Wynyard S, Nathu D, Garkavenko O, et al. Microbiological safety of the first clinical pig islet xenotransplantation trial in New Zealand. Xenotransplantation. 2014;21(4):309-323.
46. Matsumoto S, Wynyard S, Giovannangelo M, et al. Long‐term follow‐up for the microbiological safety of clinical microencapsulated neonatal porcine islet transplantation. Xenotransplantation. 2020;27(6).
47. Denner J. Why was PERV not transmitted during preclinical and clinical xenotransplantation trials and after inoculation of animals? Retrovirology. 2018;15(1):28.
48. Niu D, Wei HJ, Lin L, et al. Inactivation of porcine endogenous retrovirus in pigs using CRISPR-Cas9. Science. 2017;357(6357):1303-1307.
49. Einsiedel EF. Commentary: On the position paper of the Ethics Committee of the International Xenotransplantation Association. Transplantation. 2004;78(8):1110-1111.
50. PHS Guideline on Infectious Disease Issues in Xenotransplantation. Food and Drug Administration; 2001. (Accessed June 28, 2022 at https://www.fda.gov/media/73803/download)
51. First WHO Global Consultation on Regulatory Requirements for Xenotransplantation Clinical Trials Changsha, China, 19-21 November 2008. Xenotransplantation. 2009;16(2):61-63.
52. Welin S. Starting clinical trials of xenotransplantation--reflections on the ethics of the early phase. J Med Ethics. 2000;26(4):231-236.
53. Cooper DKC, Pierson RN, Hering BJ, et al. Regulation of Clinical Xenotransplantation—Time for a Reappraisal. Transplantation. 2017;101(8):1766-1769.
54. Hurst DJ, Padilla LA, Cooper DKC, Paris W. Scientific and psychosocial ethical considerations for initial clinical trials of kidney xenotransplantation. Xenotransplantation. 2022;29(1).
55. Hurst DJ, Padilla LA, Walters W, et al. Paediatric xenotransplantation clinical trials and the right to withdraw. J Med Ethics. 2020;46(5):311-315.
56. Cooper DKC, Wijkstrom M, Hariharan S, et al. Selection of Patients for Initial Clinical Trials of Solid Organ Xenotransplantation. Transplantation. 2017;101(7):1551-1558.
57. Yamamoto T, Iwase H, Patel D, et al. Old World Monkeys are less than ideal transplantation models for testing pig organs lacking three carbohydrate antigens (Triple-Knockout). Sci Rep. 2020;10(1):9771.
58. Kozlov M. Clinical trials for pig-to-human organ transplants inch closer. Nature. Published online July 6, 2022.
59. Montgomery RA, Mehta SA, Parent B, Griesemer A. Next steps for the xenotransplantation of pig organs into humans. Nat Med. 2022;28(8):1533-1536.